Bringing Blood Draws Closer to Home
How a Simple Change is Transforming Care for Vulnerable Patients
Innovation | Innovarium

When Soojee Sim looked at the daily schedule of patients coming through St. Paul's Hospital (SPH) for blood transfusions, she saw more than appointments – she saw unnecessary burden on s people with complex social and medical needs.
"Imagine you live so far away, and this is the provincial program, and therefore you have to travel to downtown Vancouver to see the clinicians and receive the care you need," explains Sim, clinical program coordinator at Providence Health Care (PHC).
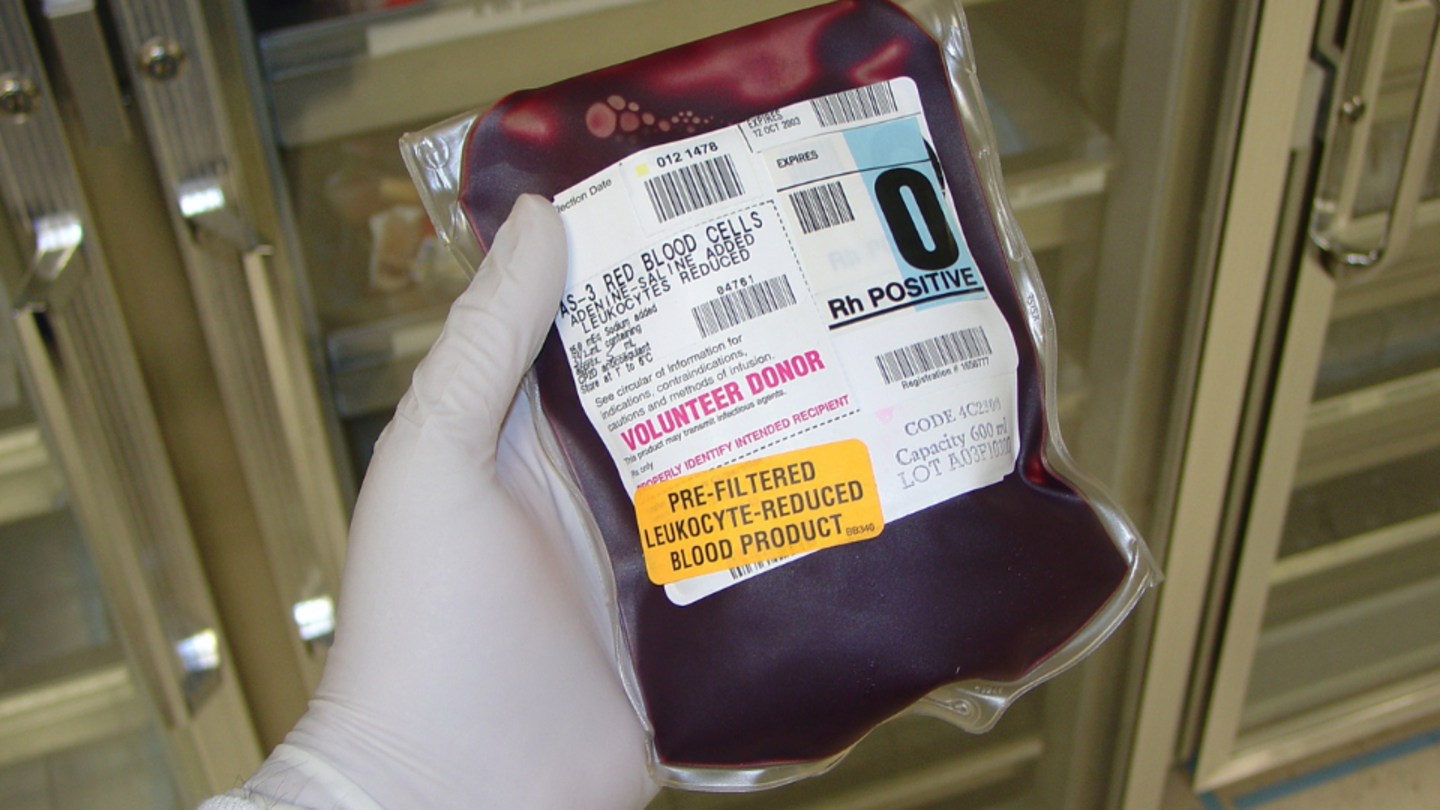
For patients with transfusion-dependent blood disorders like thalassemia, this isn't a one-time inconvenience. These patients need regular transfusions every three to six weeks to survive, requiring a complex pre-transfusion blood test called crossmatching each time.

The Hidden Burden of Red Cell Disorders
The challenges of these blood disorders extend beyond just medical symptoms. "Sickle cell disease and thalassemia disproportionately affect certain ethnic groups, contributing to disparities in health care access, socioeconomic status, and overall well-being,” explains Dr. Hayley Merkeley, Medical Director for the Adult Red Cell Disorders Program at PHC.
For these patients, the traditional process was particularly burdensome: travel to the hospital for pre-transfusion testing, return home, then travel back again for the actual transfusion – or wait hours at the hospital while labs processed their samples.
"They might have to look for childcare, they might have to miss work, or school," Sim notes. "For some patients, it may take two and a half hours on transit to get to their appointment."
A Simple but Revolutionary Idea
Sim's insight came from a surprisingly straightforward question: "The patient is actually traveling twice. Why not create a solution where the blood will travel, instead of the patient having to travel twice?"
Tina Jacobucci, team lead of the transfusion medicine lab at St. Paul's, had encountered a similar program at a conference in Toronto.
"I came back home and thought, well, could we do something here in BC?" Jacobucci recalls. "And so that's when I approached Soojee, who was working on another project with us, and just asked her, 'Hey, this is going on in Toronto. What do you think—do you think we could do this for our patients?' And she said, 'Yes, let's do it.'"

Building a Better System
With funding from the Ministry of Health Innovation Pathway Program, the team launched the Near-Patient Crossmatch Sample Collection program. They partnered with LifeLabs (a private lab company) and Fraser Health to establish community collection sites where patients could have their pre-transfusion blood work done closer to home.
The team was strategic about site selection. "We mapped out using Google Maps," Sim explains, "and actually pinpointed, without using patient identification at all. We could zoom in and identify where the density was.'"
For lab staff, the program offered relief from time-sensitive testing pressures. "Having that sample sooner, instead of the same day... allowed us to work it into our workflows better," explains Jacobucci. "When a patient comes in on the same day, we have to drop everything else we're doing. Having to deal with the additional testing that's required for these patients can be really hard on our workflows."
Overcoming Obstacles
Despite the obvious benefits, the team faced an unexpected challenge: patient hesitation.
"[Patients] love the idea, but they were scared," Sim remembers. "Imagine you always came here to get the blood collected. There's already a relationship where they’ve established trust with their health care provider, and now you're sending them somewhere where they fear they aren’t familiar with their disease at all."
The solution required personalized outreach. "We couldn't actually target everyone," Sim says. "We'd have to talk to each one: 'Are you interested? Can I tell you more about it and reassure that they're only doing the work of poking you?'"
This trust-building approach paid off. From November 2023 to March 2024, the program tracked 87 transfusions among participating patients. The time from hospital check-in to starting a transfusion dropped from over an hour to less than 20 minutes, with sample quality maintained at high standards.
The Surprise Outcome
Perhaps the most interesting finding came from an unexpected source. While pre-transfusion wait times decreased dramatically, the overall time patients spent in the unit didn't decline as anticipated. The reason? Purely social. Patients were choosing to stay longer post-transfusion specifically to socialize with others sharing their condition – a powerful reminder that health care isn't just about clinical efficiency.
"If the patients want to kind of create their own social community for each other's support... it was very hard to say, 'Okay, you guys are not supposed to socialize in here. You guys are done. You guys need to go home,'" Sim notes.
System-Wide Benefits
Beyond patient convenience, the program has created ripple effects throughout the health care system.
"The patients are not occupying the beds while they're waiting for the crossmatch to be done because their blood has already arrived," Sim explains. "That two to four hours saved on each of these patients every three to six weeks could free up resources they utilize to treat somebody else, because in MSSU (medical short stay unit), there are a lot of chemo-receiving patients and patients that are going through diagnostic procedures."
For patients, the benefits extend beyond saved time, reducing transportation costs, minimizing lost work and school hours, and eliminating additional childcare expenses.
Looking Ahead
The success of the program has generated interest across BC’s health care system. Expansion plans are already underway.
"The business proposal -- which is for PHC, Vancouver General Hospital, and Fraser Health Care Sites --went in and has been accepted, and now has been signed off," Sim reports, noting that the program will expand offering sweeping impacts to patients with a red cell disorder.
However, scaling up presents its own challenges. Standardization across health systems remains complex. As Jacobucci points out, "Even something as simple as arm banding," the use of patient identification wristbands, can vary between hospitals, with each having its own patient identification protocols.
For Sim, the key lesson isn't about the technology or even the funding – it's about collaboration. "It's not the budget that we require to do such amazing work, I think it's the like-minded people who want to create consistent goals for the patient and for betterment of people."
As health care systems worldwide grapple with efficiency and access challenges, this BC initiative demonstrates how rethinking even basic processes can transform care delivery. Sometimes, innovation isn't about developing new technologies or treatments – it's about finding smarter ways to deliver the care we already have, especially to those who need it most.